- Replies 121
- Views 3.4k
- Created
- Last Reply
Top Posters In This Topic
-
ArcticCrusher 43 posts
-
akvanden 22 posts
-
Highmark 15 posts
-
EvilBird 13 posts
Most Popular Posts
-
It always a sure sign of intellect and success when someone ends every post by calling someone a moron or idiot.
-
Or as the severity of illness the virus causes continues to weaken just treat it like the common cold.
-
Sticking with the kool-aid I see.
Featured Replies
Recently Browsing 0
- No registered users viewing this page.









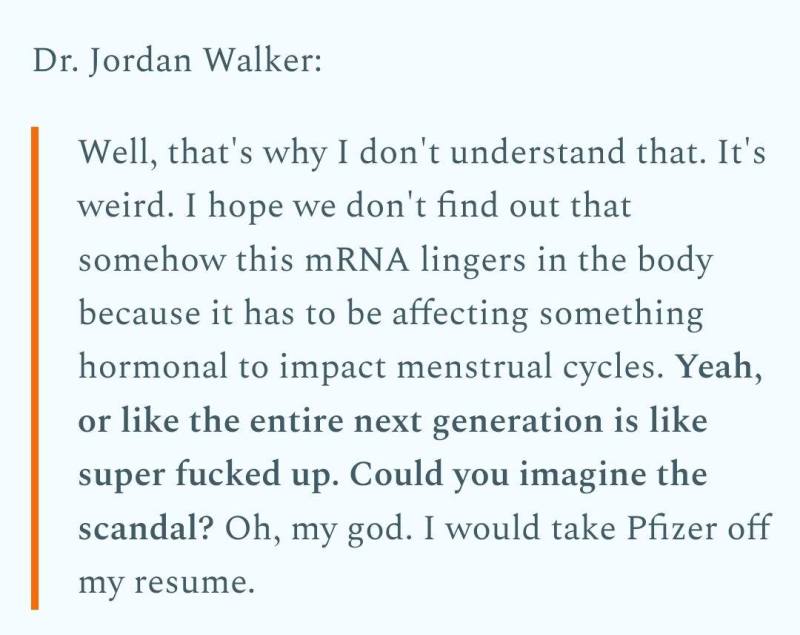

Lets not forget the mRNA jab makes the bodies immune system act like it had COVID.
Both the article and the study provide some very interesting reading on what the virus and mRNA vaccine do to the immune system.
https://slate.com/technology/2023/01/immunity-covid-research-airborne-aids-debunk.html
When the immune system goes awry, it’s bad news. A wonky immune system might mean that you’re more likely to catch colds and flus, or be infected by other pathogens—and less likely to shake them off. It might mean that your body fails to detect and destroy growing tumors. It might even mean that the body turns against itself, leading to chronic autoimmune conditions like arthritis or Crohn’s disease. The fallout of immune system dysfunction on the human body is widespread and unpredictable—which is why it was so concerning in 2020 when evidence began to amass that COVID-19 seemed to be disrupting human immunology. So much so, in fact, that John Wherry, director of the Penn Medicine Immune Health Institute, summed it up this way to Kaiser Health News: “COVID is deranging the immune system.”
Most of the early immunological evidence—the evidence that Wherry was referring to—came from patients who died or suffered severe COVID. Now, three years of infections and immunizations later, severe COVID is getting mercifully less common; a brush with the virus may well feel unremarkable. And a new idea about how COVID can affect immunity has emerged: that even mild infections routinely cause consequential damage to our bodies’ defenses. This quiet degradation was memorably termed “immunity theft” by one evolutionary biologist speculating on why this fall’s respiratory virus season seemed more severe than usual.
There are plenty of reasons to not want to get COVID over and over, but the prospect of an increasingly damaged immune system is a particularly compelling one. Throughout the pandemic, scientific evidence has mounted that mild COVID infections may be doing something to our immune systems—prompting many on social media to hyperbolically describe COVID as “airborne AIDS.” But the lessons that scientists are drawing from their research are nuanced—and the larger picture says more about the sturdiness of our collective immunity than anything else.
There are a few ways scientists can probe COVID’s impact on immune systems. One is to investigate how well the immune system can rally against a second go-round with SARS-CoV-2. At the start of the pandemic, Shane Crotty, of the La Jolla Institute of Immunology, published some of the first papers looking at the immune response to COVID. “There was a lot of concern about how strange it might look,” he said. But really, “it looks as we would largely expect for a respiratory viral infection.” Antibodies recognize and subdue the virus, while immune memory cells linger about, ready to gear up for the next infection. A similar response is seen after vaccination. Because of this robust immune response, SARS-CoV-2 infections are now, on average, shorter and milder. So far this year, COVID hospitalizations have not surged, despite high rates of infection. Some of this attenuation may be due to a meeker (arguably) omicron variant, but it’s more likely because, with respect to fending off COVID at least, our immune systems are working just as they’re supposed to.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9012513/
Vaccination has also been demonstrated to suppress both IRF7 and STAT2 (Liu et al., 2021). This can be expected to interfere with the cancer-protective effects of BRCA1 as described above. Cancers associated with impaired BRCA1 activity include breast, uterine, and ovarian cancer in women; prostate and breast cancer in men; and a modest increase in pancreatic cancer for both men and women (Cancer risk and BRCA1 gene, 2021).
Reduced BRCA1 expression is linked to both cancer and neurodegeneration. BRCA1 is a well-known breast cancer susceptibility gene. BRCA1 inhibits breast cancer cell proliferation through activation of SIRT1 and subsequent suppression of the androgen receptor (Zhang et al., 2016). In a study conducted by Suberbielle et al. (2015), reduced levels of BRCA1 were found in the brains of Alzheimer's patients. Furthermore, experiments with knocking down neuronal BRCA1 in the dentate gyrus of mice showed that DNA double-strand breaks were increased, along with neuronal shrinkage and impairments in synaptic plasticity, learning and memory.
Analysis detailed in a recent case study on a patient diagnosed with a rare form of lymphoma called angioimmunoblastic T cell lymphoma provided strong evidence for unexpected rapid progression of lymphomatous lesions after administration of the BNT162b2 mRNA booster shot (Goldman et al., 2021). Comparisons of detailed metrics for hypermetabolic lesions conducted immediately before and 21 days after the vaccine booster revealed a five-fold increase after the vaccine, with the post-booster test revealing a 2-fold higher activity level in the right armpit compared to the left one. The vaccine had been injected on the right side. It is worth pointing out in this regard that lymphoid malignancies have been associated with suppression of TRAIL-R1 (MacFarlane et al., 2005).
Over the last three decades, the mRNA technological platform aimed to develop effective and safe nucleic acid therapeutic tools is said to have overcome serious obstacles on the coded product instability, the overwhelming innate immunogenicity, and on the delivery methodologies (Pardi et al., 2018). One of the major success stories of mRNA use as a genetic vaccination tool is on the introduction of robust immunity against cancer (Van Lint et al., 2015). In addition, the potential of mRNAs to restore or replace various types of proteins in cases of rare genetic metabolic disorders like Fabry disease has offered great potential therapeutic alternatives where no other medication has proved to be successful (Martini and Guey, 2019). However, in the case of mRNA use as genetic vaccines against infectious diseases, the preliminary safety investigations seemed to be premature for a world-wide use in the general population (Pardi et al., 2018; Doulberis et al., 2021).
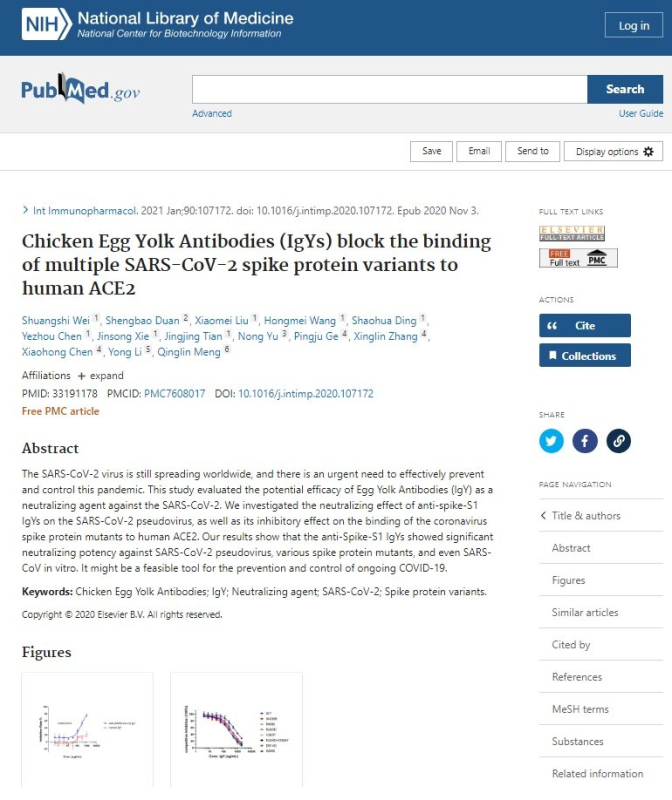
Although there are essential epitopes on other SARS-CoV-2 proteins where an antibody response could have provided essential immunogenicity, well known from SARS-CoV-1 (Gordon et al., 2020), the primary goal of the developers of the SARS-CoV-2 mRNA vaccines was to design a vaccine that could induce a robust antibody response exclusively to the spike glycoprotein. Such antibodies, especially IgA in the nasopharynx, should cause the invading viruses to be quickly cleared before they could invade host cells, thus arresting the disease process early on. As stated succinctly by Kaczmarek et al. (2021):
“The rationale behind vaccination is to provide every vaccinated person with protection against the SARS‐CoV‐2 virus. This protection is achieved by stimulating the immune system to produce antibodies against the virus and to develop lymphocytes that will retain memory and the ability to fight off the virus for a long time.” However, since vaccination is given parenterally, IgG is the principal antibody class that is raised against the SARS-CoV-2 spike glycoprotein, not IgA (Wisnewski et al., 2021).
Vaccines generally depend upon adjuvants such as aluminum and squalene to provoke immune cells to migrate to the injection site immediately after vaccination. In the history of mRNA vaccine development, it was initially hoped that the mRNA itself could serve as its own adjuvant. This is because human cells recognize viral RNA as foreign, and this leads to upregulation of type I IFNs, mediated via toll like receptors such as TLR3, TLR7 and TLR8 (Karik ó et al., 2005).
However, with time it became clear that there were problems with this approach, both because the intense reaction could cause flu-like symptoms and because IFN-α could launch a cascade response that would lead to the breakdown of the mRNA before it could produce adequate amounts of SARS-CoV-2 spike glycoprotein to induce an immune response (de Beuckelaer et al., 2016). A breakthrough came when it was discovered experimentally that the mRNA coding for the spike protein could be modified in specific ways that would essentially fool the human cells into recognizing it as harmless human RNA. A seminal paper by Karikó et al. (2005) demonstrated through a series of in vitro experiments that a simple modification to the mRNA such that all uridines were replaced with pseudouridine could dramatically reduce innate immune activation against exogenous mRNA. Andries et al. (2015) later discovered that 1-methylpseudouridine as a replacement for uridine was even more effective than pseudouridine and could essentially abolish the TLR response to the mRNA, preventing the activation of blood-derived dendritic cells. This modification is applied in both the mRNA vaccines on the market (Park et al., 2021).
Regarding SARS-CoV-2, relevant studies reveal overwhelming similarities between SARS-CoV-2 pG4s, including in RNA coding for SARS-CoV-2 spike glycoprotein, and those sequenced in the human transcriptome (Zhang et al., 2020). Thus, it can be inferred that synthetic mRNAs in vaccines carrying more pG4 structures in their coding sequence for SARS-CoV-2 spike glycoprotein will amplify and compound the potential post-transcriptional disorganization due to G4-enriched RNA during natural SARS-CoV-2 infection.
Edited by Highmark